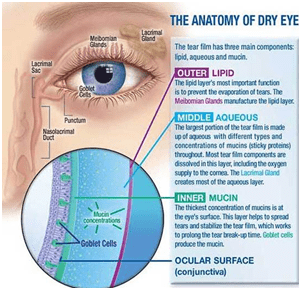
Tears are one of the body’s natural defense mechanisms. They are produced by various glands in the eye and are secreted to coat, protect and nourish the surface of your eye. Tears carry essential vitamins and nutrients across the surface of the eye. They also act as a shield against damaging factors such as wind, heat, smog or foreign particles. Normally, every time you blink, you add another protective coating of tears over the eyes whilst flushing out old tears.
Dry eye occurs when the eye does not produce tears properly, or when the tears are not of the correct consistency and evaporate too quickly.
In addition, inflammation of the surface of the eye may occur along with dry eye. If left untreated, this condition can lead to pain, ulcers, or scars on the cornea, and some loss of vision. However, permanent loss of vision from dry eye is uncommon.
Dry eye can make it more difficult to perform some activities, such as using a computer or reading for an extended period of time, and it can decrease tolerance for dry environments, such as the air inside an airplane.

People who suffer from Dry Eye experience a variety of symptoms, including:
While age is a prominent cause of Dry Eye, it can also be triggered by many other factors, including;
• Digital device use
• Preservatives contained in some bottled products for use in the eye, such as eyedrops or artificial tears. Frequent use of these products can aggravate dry eye conditions.
• Medications (antihistamines, antidepressants, diuretics, psychotropics, cholesterol lowering agents, betablockers, oral contraceptives, arthritic)
• Systemic disease (such as Diabetes, thyroid disease, rheumatoid arthritis, systemic lupus erythematosus, rosacea, hepatitis C infection, HIV infection, Sjogren’s syndrome, sarcoidosis) can lead to abnormal tear production
• Age (weakened immune system)
• Gender (post menopausal females are a large risk group due to decrease in hormonal levels leading to loss of anti-inflammatory protection)
• Poor diet (low water intake, excess caffeine and/or alcohol intake, low amounts of fatty acid intake etc)
• Asian ethnicity
• Heating/cooling systems (decreased humidity)
• Hormonal changes (chronic androgen deficiency, menopause and hormone replacement therapy)
• Cancer treatment (systemic chemotherapy, radiation therapy)
• Previous eye surgery (such as LASIK, refractive surgery, corneal transplantation)
• Previous eye injury (eg chemical burns) or infection
• Irregularities of the conjunctival surface (outer white layer of eye) such as pingeculae or pterygia
The only way to know for sure if you’ve got chronic dry eye syndrome is to have your eye doctor perform one or more dry eye tests during an eye exam.
Symptoms alone are poor predictors of the presence and severity of dry eye disease. Symptoms can vary significantly from person to person.

While there is no known cure for Dry Eye Disease, you can relieve the symptoms of dry eye. Most eye care practitioners recommend artificial tear products (ocular lubricants) for their patients with Dry Eye. To help ease symptoms of Dry Eye some simple measures can be taken such as
First line of action:
1. Wear glasses when you are outdoors to help keep out wind, glare and dust
2. Avoid spending prolonged periods in air-conditioned or heated environments as this can cause a higher rate of evaporation, resulting in dry eyes.
3. Consider using a cool-air mist humidifier at home.
4. Avoid smoking, and avoid smoky environments
5. Get plenty of sleep
6. Eat more fresh fruit and vegetables, particularly foods rich in Vitamin A, C and E.
7. Reduce the intake of processed, salty or deep fried foods to maintain a healthy balanced diet.
8. Liquid consumption: Drink the equivalent of 8-10 glasses of water (~2L) per day to keep the body well hydrated.
9. Avoid beverages and foods which have diuretic effects such as coffee, caffeinated teas (less than 2 cups), alcohol (less than 1 standard drink) etc.
10. Nutritional supplements: foods rich in Omega-3 fatty acids may decrease ocular surface inflammation. Dietary sources of Omega-3 include fatty fish, such as Sardines ( ‘Mathi’) salmon and tuna(‘Choora’). Flaxseed Oil or Chia Seed are suitable vegetarian alternatives.
11. Discuss with your ophthalmologist about the possibility of altering or decreasing the use of medications that can lead to dry eyes. Common culprits are antihistamines and antidepressants.
12. Whilst reading, watching television or working on the digital devices (computer screens, tablets, mobile phones), remember to consciously blink frequently and take regular breaks( 20 -20 rule 20 mins work followed by 20 secs break ).
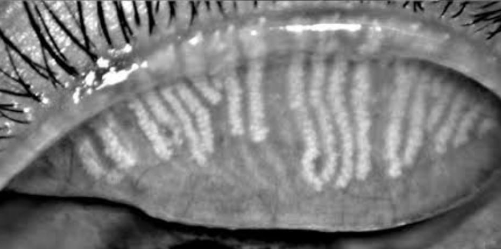
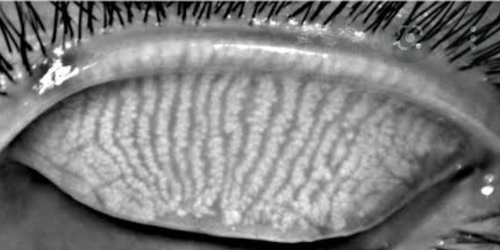
13. Tears evaporate very quickly if there is not enough oil covering the tear layer. There a few things you can do.
a. Use sterile warm compresses on closed eyes for 8mins followed by eyelid massaging for 2mins, to help loosen any blockages in the oil glands
b. Refrain from using tap water to clean eyes.
c. In some cases, an antibiotic (eye drop/ointment) is prescribed to reduce the bacterial population in the eye area. Excess bacteria can lead to evaporative dry eyes, as they break down the oily layer of the tear film.
d. Use tear supplements for dry eyes. Where possible, choose non-preservative options for lubricants.
e. In severe Dry Eye, you may be asked to instil an additional eye gel .These will apply a thick coating over the eye’s surface to keep it moist and reduce evaporation whilst you sleep.
Second Line of action
1. Is Under Supervision of your treating Ophthalmologist. The doctor will decide whether antibiotic drops or ointment is needed (If the eye shows Cronic Infection)
2. Immune – Suppressing drop may have to be use to reduce inflammation in collagen Diseases.
3. Topical Anti Inflammatory drops may be used in some cases; but Reduced after cataract surgery as it may worsen dry eye.
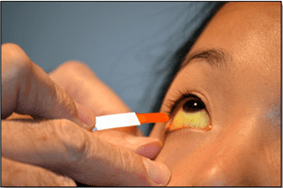
4. Punctal occlusion uses a silicone plug to decrease loss of tears through the drainage system, keeping more tears on the ocular surface. It acts like a stopper placed in a drain of a sink.
5. Moisture chamber spectacles are not popular in India
6. Secretagogues – they help increase production of tears in the lacrimal gland

Third Line of action
1. Autologous serum eyedrops (ASEDs) – are eyedrops made using a patient’s own blood.
2. Therapeutic contact lenses – extended wear silicone-hydrogel contact lenses
3. Permanent punctal occlusion – thermal cautery is done to permanently seal the drainage hole.
4. Mucolytic therapy – if mucous strands or filaments cause severe discomfort, topical N-acetylcysteine
Fourth Line of action
1. Systemic anti-inflammatory medications
2. Surgery (lid surgery, tarsorrhaphy; mucous membrane, salivary gland, amniotic membrane transplantation).
Call us
Call us
Call us
Get Direction
© 2024 Roshan Eye Care, All Rights Reserved.
Looking for a website? Let it be a company website or a portfolio one, we got you covered. Let’s talk about your requirements or something about that brewing web idea in your mind.